Panel Discussion: 1

Clinical Applications of Next-Generation Sequencing in Precision Oncology
The panel members included: Dr. Saadvik Raghuram, a renowned oncologist at Medicover Cancer Institutes who completed his MBBS from JSS Medical College and DM in Medical Oncology and MD in Radiation Oncology; Dr. Vamshi Krishna, AIG Hospitals; Dr. Sudha Sinha, CARE Hospitals; Dr. Shrikar Kumar, Onco Cancer Centres; and Dr. Chinnababu Sunkavalli, Yashoda Hospitals.
The discussion started off with Dr. Kalyan greeting all thepanelists. Dr. Kalyan was the moderator of the session. Thediscussion was about the landscape of what cancertreatments were going to be in the future and howmolecular testing would play a role in the diagnosis, testing,and management of the disease.
Increasing Incidence of Cancer and Scope of Screening
The first topic of the discussion was the increasing incidence of cancer, the scope of screening, and what capacity building could be done to improve screening. The initial views were given by Dr. Chinnababu, whose main focus is cancer screening and prevention. Dr. Chinnababu also runs the Grace Cancer Foundation, which he has been running for nearly 20 years and has had an impact in nearly 130 countries.
Dr. Chinnababu expressed his happiness to share his on-ground experience over the last decade on community screening. Dr. Chinnababu mentioned that, looking at various data from Globocan and other sources, the incidence of cancer has in fact been increasing in low- and middle-income countries. Looking at the USA, the incidence of cancer has been declining by 1.3 % every year, whereas in this part of the world we see around 20 lakh new cases per year.

Most Common Cancer in Hyderabad
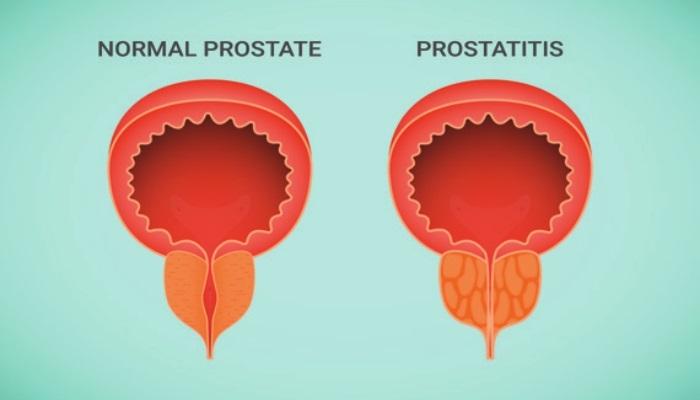
In our part of the world, head and neck cancers are more common, as are gastric and lung cancers in men and breast and cervical cancers in women. Hyderabad was seen as having more breast cancer cases than any other district. The increase in the incidences can be attributed to increased awareness and improved screening methods for early detection. The community engagement through mobile screening methods for oral, breast, and cervical cancers adopted by them has led to good pick-up percentages of about 1.6 percent, which is high since we are probably dealing with high-risk people compared to the US, where detection of breast cancer through mammography is 0.3 percent. Dr. Chinnababu also mentioned the “4:4:80” factor, which is made up of four lifestyle factors that can be changed: tobacco use, lack of physical activity, an unhealthy diet, and excessive alcohol consumption. These factors lead to four noncommunicable diseases: cancer, diabetes, heart disease, and pulmonary disease, which account for 80% of noncommunicable deaths and can be avoided through lifestyle changes, according to the doctor. The problem is mainly attributed to a lack of awareness. The screening rate for breast cancer in urban India is 0.5%, let alone in rural India, which is much lower, so there is a lot of scope to increase awareness and screening. Dr. Kalyan also agrees with Dr. Chinnababu that the need for screening is important and, access and capital for screening should be worked on and promoted more.
We are Living in Two Indias
Dr. Sudha, who worked in the US and also contributed to non-profit hospitals and was active in research, was the next speaker on the panel. She speaks about the rise in molecular testing and Next-Generation Sequencing (NGS) for the detection of cancer and mainly solid tumors, but there is an argument contrary to that about them being expensive and not affordable to a large percentage of people.

Considering these scenarios, Dr. Sudha was asked about the future of cancer care and when molecular tests would become a standard of care in cancer treatment and management. Dr. Sudha feels that there are two Indias, where one section can go on par with whatever is happening abroad by getting the molecular testing like NGS, etc. and also the medicines, and it is exciting depending on the accessibility and is already relevant in this age as it is available in a few hospitals. Few patients have the resources to get them done, so we do not need to wait 30 years for it to become relevant.
Coming to other parts of India is a different story, but it will happen soon when the prices will be affordable for most of the patients. About the question on if it is really an effective medicine in today’s world of oncology, Dr. Sudha feels that since targeted therapies and testing are used mostly for palliative therapies, they would be more useful if they could be used at earlier stages of cancer as well.
Relevance of Molecular tests and Palliative Therapy
The next point in the discussion was addressed by Dr. Vamshi.
Dr. Kalyan asked Dr. Vamshi about the relevance of molecular tests and palliative therapy in the context of tumor-agnostic therapy, which is treatment based on the approval of mutations regardless of the type or origin of the cancer. Dr. Vamshi states that the approach to cancer now is not just naming the cancer but also looking at it at the individual patient level. Even though there are classes of medicines for a type of cancer, there is a transition towards personalized medicine, where we are trying to sequence the tumour to find out what is making that particular tumor tick and how to attack the tumor. Personalized medicine was unheard of just five years ago, but it is now in use, and things are changing. As of now it may be used mostly for a niche set of patients, but in around 3 years’ time it would be used more regularly used. Dr. Vamshi also discussed how a study from Tata Memorial Hospital provides an example of such an approach, in which a medicine used in Indian patients at a dose one-tenth of what it was used for in patients from the United States was shown to be effective here as well as cost-effective. As a result, evidence supported by data from our population should be considered as a strategy.

Cost of Sequencing to Come Down in the Future
To add on to Dr. Sudha and Dr. Vamshi’s points, Dr. Kalyan is hopeful that the cost of sequencing is going to come down drastically because the patent of Illumina is expiring, so there will be a lot of companies coming in with their sequencing machines and most of the reagents. We’ll know more once the prices drop and this becomes the standard. What works for Caucasians may not be the only standard of care, so we need to have our own data.
The Promise of Immunotherapies
The next question was directed at Dr. Saadvik Raghuram about a promise about a trial where it cured 100 percent of colon cancers, the promise of immunotherapies, and his experience in this regard. Dr. Saadvik mentions that initially, when it started in India, most of the time it was not used in the first line setting but more in the later line setting. The results were also disappointing, and the high costs led to a debate about whether they were literally worth it, but then it all depended on where you wanted to incorporate immunotherapy into your treatment schedule. It will be better if you start in the earlier stages of cancer, combining it with chemotherapy and appropriate methods of testing.
As of now, we know that immunohistochemistry (IHC) is one method where we test to know whether a therapy works or does not work for a particular patient, which is an area of unmet need because that is not the sole modality. Despite the fact that many patients test positive for IHC, many do not respond, which brings us back to genomics, where T cells respond better to immunotherapy in tumors with genomic mutations such as ATMRB1, etc., and where the tumor environment is more inflammatory with a high concentration of NK cells. Certain kinds of mutations, even when IHC scores are pretty positive, don’t respond to immunotherapy.
Though there is really good data going forward for immunotherapy, genomics will also play a huge part in it because you need to integrate both, not only one modality of testing, but going forward we’ll be getting more data about the genomic aspects of this as well. As Dr. Sudha mentioned, immunotherapy is very expensive in India, with the most basic one costing around Rs. 1 lakh per month on average and rising to around Rs. 3-5 lakhs depending on the molecule used. So, she was hopeful, we’ll get generic versions, and they’ll be available to an increasing number of Indians once the patents expire.
Liquid Biopsy – A Diagnostic Tool
Dr. Kalyan mentions another technology that is really moving forward in terms of diagnostic help and a tool that is even easier for the patient to use: liquid biopsy. It entails testing and reporting on circulating ctDNA, which is done through sequencing, which is also an expensive test. As a result, Dr. Shrikar was asked what he thought about his clinical experience with liquid biopsies.

Dr. Shrikar mentions that it should be taken contextually. If you are looking at metastatic lung cancer in the first-line setting, there is broad approval that liquid biopsy, which is the plasma-first approach, is an accepted way of testing for your actionable genomic biomarkers. If the plasma-first approach fails to find a targeted biomarker, then you do a reflex tissue test because that allows you to do PD-L1 IHC. At the same time, if it’s in the second-line setting, the advantage of a tissue biopsy is that it is the only way you can pick up a histological transformation, something that a liquid biopsy cannot do.
If the patient can afford it, a liquid biopsy is definitely preferable, and we will decide on further testing based on the results. Looking at colon, the first phase 3 dynamic trial published recently in the New England Journal specifically looked at cell-free DNA testing in an adjuvant setting for stage 2 colon. T3, T4, and node-negative colons were tested post-surgery and then randomly assigned to adjuvant chemotherapy based on the cell-free DNA versus standard management based on the clinical low-risk and high-risk criteria. The trial demonstrated that by using liquid biopsy, it is possible to reduce chemotherapy rates by half, from 30% to 15%. But there were several flaws in that study; the methodological design is criticized, and even those patients who were ctDNA negative were clinically at high risk, and around 15 percent of them recurred at three years.
Hence, it is a little too early as far as adjuvant therapy decision-making in the colon is concerned. However, for lung cancer, liquid biopsy is the current standard, both in the first line, where it was first shown to be promising, and in the second line, which distinguishes those who have progressed on the EGFR first generation innovators and where attempting to detect the T790M mutation is the current standard.
Future Complexities of Oncology Testing
Dr. Kalyan wanted everyone to discuss two points when he spoke about how oncology practise has changed from single-line testing, such as performing a biopsy and sending it for pathology, to now requiring multiple tests in addition to multiple markers: if they anticipate that each and every cancer will become a specialty unto itself, and the second part being what skills in terms of human skill are needed in handling these in situ hybridizations, which are highly technician dependent. How much more complicated will it become as we move forward?

Dr. Sudha feels that the futuristic version that everybody gets excited about, where you have some kind of chip technology to know the exact drug response to a specific mutation at one go, which won’t happen that soon. Although it’s a really exciting time to be in oncology, we have barely scratched the surface and gotten most of the low-hanging fruits. We’ve got most of them, like the mutation, targeted therapy, response rate, and the drug that goes with it.
Living with Cancer as a Chronic Illness
Then come the more complicated ones, which are regular cancer patients, because the human body and cancer are much more complex than that, but hopefully we will reach a place where cancer will at least becomes a chronic disease, something that you will be able to live with like we are living with cardiovascular disease at least after 20 years. Dr. Sudha tries telling that to her ovarian cancer patients, but it is still not that way. She also feels that maybe with the technology that we have, you are able to achieve chronic disease for cancer, which would be a very big victory.
Dr. Chinnababu feels the same way, because “you know, even as we talk about breast cancer survival rates, we talk about 10-year survival rates, so in that way, you know the ovary has become a chronic disease.” Dr. Chinnababu also sees tremendous progress even in the surgical sphere, because now we have robotic surgery taking up a significant part of oncology practice, and in the days to come, you will also have nanorobots and other amazing technologies shaping the way we practice. It is also exciting because of electronic health records and the digitization of digital healthcare, as well as the tremendous potential for real-world evidence for the outcomes that we have, particularly when discussing targeted therapies.
Dr. Chinnababu feels the same way, because “you know, even as we talk about breast cancer survival rates, we talk about 10-year survival rates, so in that way, you know the ovary has become a chronic disease.” Dr. Chinnababu also sees tremendous progress even in the surgical sphere, because now we have robotic surgery taking up a significant part of oncology practice, and in the days to come, you will also have nanorobots and other amazing technologies shaping the way we practice. It is also exciting because of electronic health records and the digitization of healthcare, as well as the tremendous potential for real-world evidence for the outcomes that we have, particularly when discussing targeted therapies.