Hyperthyroidism and Precision Medicine: Diagnostic Issues

Thyroid hormones play an integral role in our physiology – they regulate metabolism, cardiovascular and bone health, neurological functions, and body growth. Aberrations in thyroid hormone levels impact almost all major body systems. Thus, early diagnosis and management of thyroid disorders is extremely important.
Precision medicine is vital to determine specific environmental and genetic factors that increases risk of thyroid disorders and affect treatment outcomes. This can help to diagnose and treat thyroid dysfunctions better by using tailored treatment strategies. In this article, we shall discuss the problems pertaining to diagnosis of hyperthyroidism using precision medicine.
Issues with measuring thyroid hormones
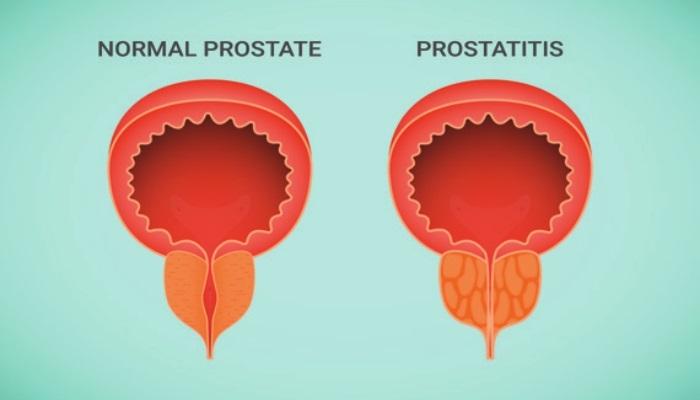
Serum TSH levels is the key for diagnosis of thyroid dysfunction. Unfortunately, there are quite some issues related to the assessment of TSH levels :
- TSH cross-reacts with other glycoproteic hormones which can result in falsely elevated TSH levels, (this problem can be countered by using monoclonal antibody assays).
- Endogenous TSH antibodies and inactive forms of TSH can affect TSH levels.
- Other factors like time of TSH sampling, drugs, body weight, pregnancy can all affect TSH levels
For measuring serum T3 and T4 levels, we have developed highly reliable and accurate technology like liquid chromatography tandem mass spectrometry. However, the issue is that we still follow the standard reference values completely obliviating the fact that there are individual factors that affect thyroid hormone levels and ‘normal’ T3 and T4 values are patient specific.
Diagnostic challenges in Grave’s disease:
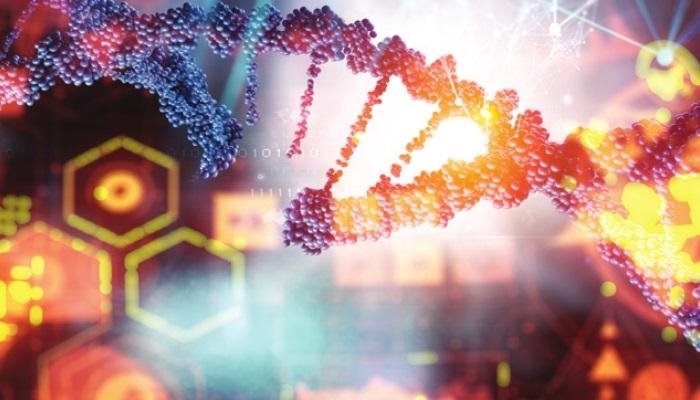
Twin studies have shown that Grave’s disease may be triggered by genetic predisposition. Specific genotypes of HLA,CTLA4,CD40 and thyroglobulin may contribute to Grave’s disease. However, we are yet to figure out the specific combination of genetic variations that causes this condition.
Grave’s disease is diagnosed by the presence of antibodies (Ab) against the TSH receptor (TRAb). Some patients having hyperthyroidism and diffuse goiter have undetectable antibody levels whereas some patients with detectable TRAb levels have silent thyroiditis and not Grave’s disease. Such issues may lead to inaccurate diagnosis.
Limitations and difficulties in Precision medicine
Personalized or precision medicine requires a large amount of information in the form of clinical data, laboratory investigations, behavioral and psychosocial data, and biological information etc. This data would then have to be analyzed to address questions related to the prevention and treatment of thyroid dysfunction. In a nutshell, it would require a huge investment of time and money.
Other Systemic Chemotherapy Toxicities
Commonly reported systemic toxicities during breast cancer chemotherapy include nausea, vomiting, diarrhea or constipation, pain, arm swelling, breast skin irritation, and high susceptibility to infections. One study found an SNP, calcium channel voltage-dependent subunit beta 4 (CACNB4), which was associated with docetaxel-induced alopecia. Different pharmacogenomic studies have determined various chemotherapy-associated toxicities in breast cancer patients, but they were not consistent in their selected outcome, their selected genes, and the used chemotherapeutic regimens.
Other barriers in the way of development of precisionmedicine tailored for hyperthyroid treatment includes hightesting cost, lack of reliable biomarkers that can predictmost conditions, and insufficient knowledge among theclinicians regarding genetics and genetic counseling withregards to thyroid disorders.

Reference:
1. Elsevier. Volume 63, Issue 7. Pages 354-363. (Aug-Sept, 2016). https://www.elsevier.es/en-revista-endocrinologia-nutricion-english-edition–412-articulo-thyroid-dysfunction-in-era-precision-S2173509316300745. Accessed on August 10, 2022.
2. PubMed. Bioinformatics challenges for genome-wide association studies. Feb 15, 2010; 26(4): 445-455. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2820680/. Accessed on August 10, 2022.
3. Paul W. Ladenson. Precision medicine comes to thyroidology. The Journal of Clinical Endocrinology & Metabolism, Volume 101, Issue 3, 1 March, 2016. https://academic.oup.com/jcem/article/101/3/799/2804722. Accessed on August 10, 2022