Pharmacogenomics of methotrexate in patients with Rheumatoid arthritis – Current Knowledge and Challenges

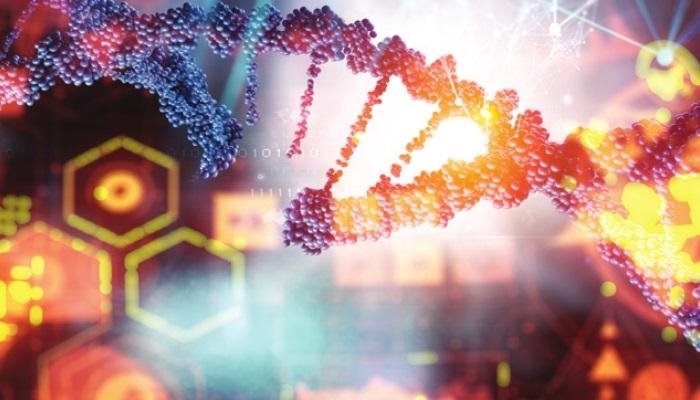
Genetics play a huge role in determining disease activity and treatment response. In this era of precision medicine, genotyping has become extremely important to identify the safest, effective, and cost-effective treatment.
Methotrexate(MTX), a conventional synthetic DMARD, is a potent anti-inflammatory and antiproliferative drug and the gold standard for the treatment of RA. However, around 30-40 % of the patients who take MTX do not get relief and eventually discontinue treatment owing to its adverse effects like nausea, oral ulcers, abdominal distress, fatigue, chills, dizziness, etc. This disparity in MTX effectiveness can be partly explained by understanding the pharmacogenomics of this drug.
In this article, we shall investigate how long we have come to understand MTX pharmacogenomics and what are the challenges in incorporating this data in clinical settings.
Genetic biomarkers of MTX response:
-
MTHFR: Methylenetetrahydrofolate reductase (MTHFR) is probably the most widely studied gene in RA. This gene encodes an important enzyme that catalyzes various reactions in the MTX cellular pathways. Studies show that:
- Patients having MTHFR 1298AA and MTHFR 677CC genotype show better clinical improvement with MTX.
- MTHFR677TT carriers have more than 4-fold risk for nonresponse to MTX when compared to MTHFR677C carriers.
-
ATIC: ATIC is an important gene involved in the metabolism of MTX. Studies have shown that:
- ATIC 347CC genotype is associated with high MTX efficacy.
- ATIC 347GG genotype is associated with high risk of gastrointestinal adverse effects related to MTX.
- ATIC 347 GG+GC genotype is associated with lack of response to MTX and MTX related toxicity in Caucasian patients with RA.
-
MTX transporters: RFC-1 80G > A is a folate transport protein with high affinity to MTX.
- People with RFC1 80A allele (AA-GA) respond better to MTX than those with the RFC1 80 GG genotype.
- Patients with RFC-1 AA genotype respond better to MTX therapy than carriers of AG and GG genotypes.
- MTR / MTRR : MTR and MTRR enzymes participate in folate and adenosine metabolism. MTR AG and MTRR G allele have been found to show poor response of MTX in RA patients.
- Thymidilate synthase: Thymidilate synthase (TS) is a folate pathway enzyme that is inhibited by MTX polyglutamates (MTX is converted to MTX polyglutamates in the cell). Patients having ‐3R allele of the genetic variant in the enhancer region of thymidylate synthase which encodes TS (TYMS‐TSER‐2R/3R) have higher TYMS mRNA expression than those with ‐2R and require a higher MTX dosage.
MTX pharmacogenomics research challenges

In the past few decades, a lot of research has been done related to methotrexate pharmacogenomics in RA. However, using these research data in clinical decision making is still a challenge due to the following reasons:
- The genetic biomarkers of MTX discussed in this article lack a strong evidence base that supports its use in personalizing care.
- Although, the genetic biomarkers of MTX are good predictors of drug effectiveness, they still don’t fully explain the patient response to treatment.
- Various factors such as sex, ethnicity, RF status, duration of the disease and treatment, prescribed dose of MTX, MTX with or without the combination of other drugs and even the baseline disease activity of the participants in the pharmacogenomic studies might greatly influence the correlation of genetic polymorphisms and the MTX efficacy.
These challenges can be tackled. Ideally, the only way to tackle these challenges is to conduct high quality research with large sample sizes, homogenous samples, well designed strategies to minimise bias and implementing standardized, well monitored treatment protocols.

Reference:
1. Qiu, Q., Huang, J., Shu, X. et al. Polymorphisms and Pharmacogenomics for the Clinical Efficacy ofMethotrexate in Patients with Rheumatoid Arthritis: A Systematic Review and Meta-analysis. Sci Rep 7,44015 (2017).
2. Conti V, Corbi G, Costantino M, De Bellis E, Manzo V, Sellitto C, Stefanelli B, Colucci F, Filippelli A. Biomarkers to Personalize the Treatment of Rheumatoid Arthritis: Focus on Autoantibodies and Pharmacogenetics. Biomolecules. 2020 Dec 14;10(12):1672.
3. Acosta-Herrera M, González-Serna D, Martín J. The Potential Role of Genomic Medicine in theTherapeutic Management of Rheumatoid Arthritis. J Clin Med. 2019 Jun 10;8(6):826