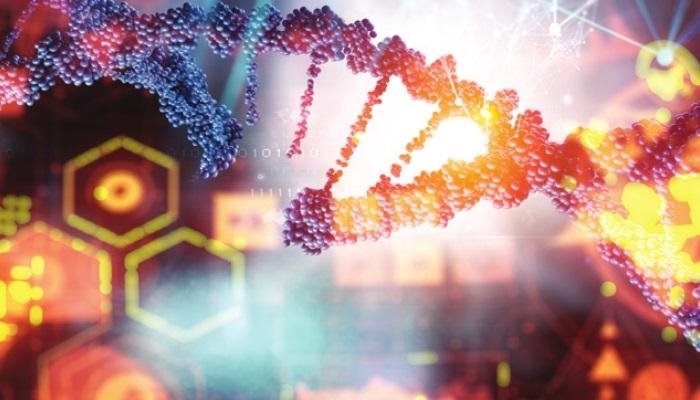
Pharmacogenomic Testing Reduces the Need for Prescription Medicines in Major Depressive Disorder

A recent trial found that pharmacogenomic testing for drug-gene interactions in patients with Major Depressive Disorder (MDD) reduced prescription of medications with predicted drug-gene interactions compared with usual care. The results of this study were published in the Journal of the American Medical Association (JAMA).
The current practice of selecting effective antidepressants for MFF has remission rates of about 30% at the initial treatment. This pragmatic, randomized clinical trial aimed to determine whether pharmacogenomic testing affects antidepressant medication selection and its clinical outcomes. The remission of depressive symptoms in the pharmacogenomic-guided group (n = 966) and the comparison group, which received usual care and access to pharmacogenomic results after 24 weeks (n = 978), were measured by the Patient Health Questionnaire-9 (PHQ-9) (remission was defined as PHQ-9 ≤ 5).
The risks for receiving an antidepressant with none, moderate, and substantial drug-gene interactions were predicted as 59.3%, 30.0%, and 10.7% in the pharmacogenomic-guided group, compared with 25.7%, 54.6%, and 19.7% in the usual care group. The remission rates over 24 weeks were higher among patients whose care was guided by pharmacogenomic testing than those in usual care, but the difference was not statistically significant.
Based on the findings of the study, it was concluded that patients with MDD had a reduced need for prescription medicines with drug-gene interactions if they were under a provision of pharmacogenomic testing under drug-gene interactions.
- Lack of awareness
- “Family First” attitude
- Reluctance to visit a doctor