Update on Chimeric Antigen Receptor (CAR) T-cell Therapy
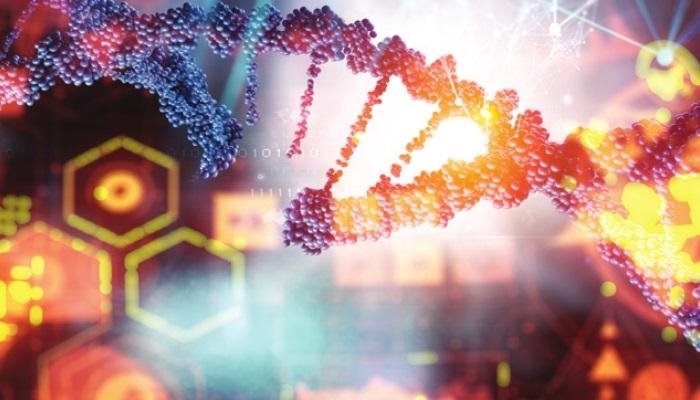
Surgery, chemotherapy, and radiation therapy have been the cornerstones of cancer treatment for many years. These continue to be the mainstream treatment methods; however, new categories of treatment have recently helped physicians around the world paint a different picture of cancer treatment for people.
Over the past decade, immunotherapy, has become what many call the “fifth pillar” of cancer treatment. This is because, in some people the immune system boosting drugs have shown remarkable ability to shrink, even eradicate the tumors at advanced cancer stages. Reportedly, in fewer cases this treatment response has also managed to last for longer years.
CAR T-cell therapy, another form of immunotherapy, has shown promising results in treating cancer and has attracted wide attention and curiosity among the cancer researchers. They are not widely used as immune checkpoint inhibitors, but have demonstrated the same capacity to destroy extremely advanced leukemias and lymphomas as well as to deter cancer for an extended period of time.
The Food and Drug Administration (FDA) has authorised six CAR T-cell treatments since 2017. All of them have been given the ‘go-ahead’ to treat blood diseases such lymphomas, some varieties of leukaemia, and most recently multiple myeloma.
In Glioblastoma (GBM):
GBM is an aggressive type of cancer that occurs in the brain or spinal cord. This therapy has shown dramatic responses in the treatment of hematologic malignancies. However, brain tumours are still considered difficult to reach.
Recent clinical trials suggest that – lack of specific tumour target antigens, tumour heterogeneity, inadequate CAR-T cell trafficking to tumour sites, T cell exhaustion (intrinsic T cell dysfunction) and the immunosuppressive microenvironment (extrinsic T cell dysfunction) of central nervous system (CNS) tumours – are the major challenges for CAR-T cell immunotherapy in treatment of GBM.
On Current state of science of commercially available CAR-T products:
CAR-T products – Tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) received approval in 2017 for the treatment of B-cell precursor acute lymphoblastic leukemia in pediatric and young adult patients, and relapsed or refractory diffuse large B-cell lymphoma after two or more lines of systemic therapy in adult patients, respectively. Additional indications have since been approved, and new agents are in development.
Among the haematological malignancy indications currently being evaluated, refractory or relapsed multiple myeloma is the most promising. Late-stage clinical trials evaluating the use of CARs targeting the B-cell maturation antigen protein found on the surface of multiple myeloma cells show efficacy in achieving durable responses with toxicity profiles consistent with leukemia and lymphoma indications proven to be viable.
Solid tumours exhibit a more complex arrangement of surface proteins, making it more difficult to find common targets for CAR. Other solid tumour indications currently being investigated in clinical trials include neuroblastoma, glioblastoma, glioma and hepatocellular carcinoma. These tumours have identified target antigens or protein expression such as EGFRvIII, GD2 and Glypican-3 that may target CAR.
Although most of the CAR T-cell infusion products are delivered via IV, studies continue to evaluate intraventricular administration for brain tumour indications and direct administration to the tumour site, such as for hepatocellular tumours.
Remodelled CAR T-cell Therapy:
As effective as CAR T-cell therapy works for some advanced cancers, it can also cause life-threatening side effects. Examples of side effects include – releasing large amounts of cytokines into blood, serious side effects on the nervous system, allergic reactions, and weakened immune system. Therefore, in 2017, NCI researchers tweaked their original CAR T-cell design with the goal of creating a safer and more effective therapy.
According to the first clinical trials, it was reported that the new therapy caused fewer neurologic side effects than the original therapy, yet showed equal efficacy. The protein CAR in the original design was replaced by two sections in the new design—called the hinge and transmembrane domains. Another section is that a protein fragment found in mice was replaced with a similar fragment found in humans in the new design. In the study, it was found that cytokine levels were lower in the blood of patients with new design therapy, hence the reduced neurologic side effects.
Another issue with the original design therapy was that the CAR T-cells did not stick longer in the blood of the patients. This could be because human immune system saw mouse proteins as unfamiliar and destroyed CAR T-cells. This issue was fixed in the new design – as it was replaced with human proteins, the patient’s immune system ignores a CAR made of human proteins, thus making the CAR T-cells stay longer. However, with reduced neurologic toxicity, and longer stay of CAR T-cells, the new CAR T-cells did not increase in efficacy.
Other clinical trials are testing CAR T-cell therapies that have been redesigned to be safer, also evaluating them in another type of blood cancer and multiple myeloma.
CAR T-cell therapies are now widely used in many countries including the United States, for the treatment of aggressive lymphomas. They have become a part of the modern medicine.
- Lack of awareness
- “Family First” attitude
- Reluctance to visit a doctor
References
- CHIMERIC ANTIGEN RECEPTOR (CAR) T-CELL THERAPY. Leukemia and Lymphoma Society. https://www.lls.org/treatment/types-treatment/immunotherapy/chimeric-antigen-receptor-car-t-cell-therapy (Accessed on 13-10-2022)
- CAR T-cell Therapy and Its Side Effects. American Cancer Society. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy/car-t-cell1.html (Accessed on 13-10-2022)
- Remodeled CAR T-Cell Therapy Reduces Side Effects in First Clinical Trial. National Cancer Instititue. https://www.cancer.gov/news-events/cancer-currents-blog/2020/car-t-cell-therapy-lymphoma-reduced-side-effects (Accessed on 13-10-2022)
- The update of chimeric antigen receptor-T cells therapy in glioblastoma. Journal of Chinese Medical Association. https://pubmed.ncbi.nlm.nih.gov/32217989/ (Accessed on 13-10-2022)
- CAR T-Cell Therapy: Update on the State of the Science. Oncology Nursing Society. https://www.ons.org/cjon/23/2/supplement/car-t-cell-therapy-update-state-science (Accessed on
13-10-2022) - Recent findings on chimeric antigen receptor (CAR)-engineered immune cell therapy in solid tumors and hematological malignancies. Stem Cell Research & Therapy.
https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03163-w (Accessed on 13-10-2022)