Use of Cardiac Drugs following Genotype Testing

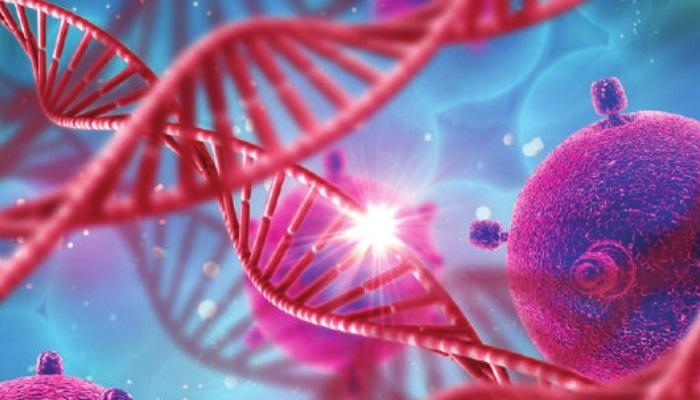
Genetic testing in Cardiovascular Diseases
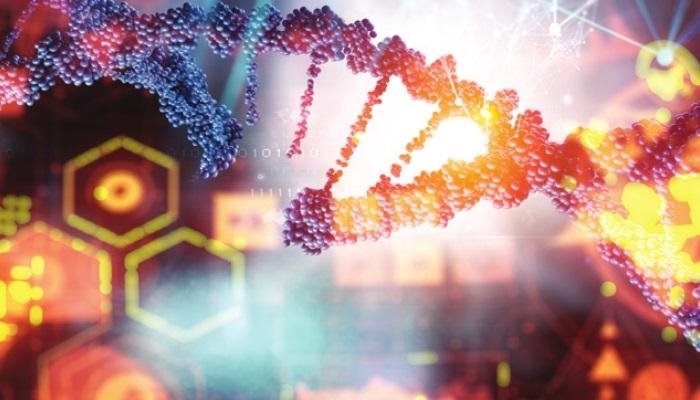
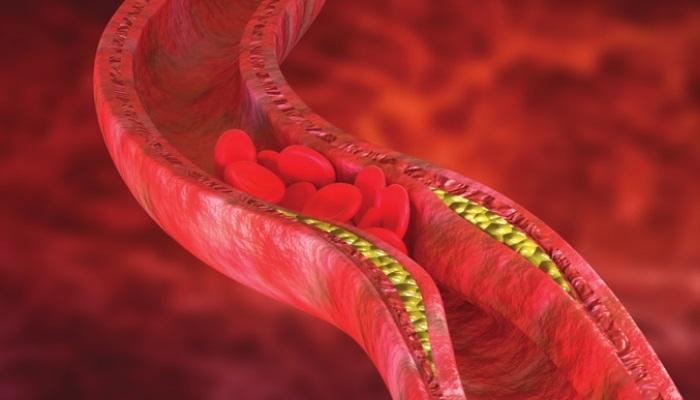
Genetic testing in cardiovascular diseases generally involves a blood test and screening of susceptible genes to identify individuals who have an increased risk for developing cardiovascular diseases (CVD) like vein thrombosis, hyperlipidemia, or atherosclerosis. A few of the genes associated with cardiovascular disorders include LDLR, APOB, PCSK9, RYR2, KCNQ1, KCNH2, SCN5A etc. Genetic testing of drug metabolism and response has contributed to the development of cardiovascular precision medicine.
Cardiovascular Drug-Gene Pairs implemented in Clinical Practice
Cardiovascular disease medications are influenced by drug responses that are genetically determined. Some of the cardiovascular drug-gene pairs with the most evidence-supporting implementation in clinical practice are listed below.
Warfarin—CYP2C9/VKORC1 genotype: Warfarin is primarily used for heart valve disease. As it interacts with other medications, the dosage is closely monitored by the physician. The combination of CYP2C9 and VKORC1 genotypes are the basis for heterogeneity in warfarin dosing. The CYP2C9 gene is involved in the clearance of S-warfarin, and genetic variation in the VKORC1 gene regulates the oxidation state of vitamin K which is associated with different sensitivity to warfarin. As a result, individuals having CYP2C9 genotype which leads to decreased drug clearance and VKORC1 genotype resulting in increased drug sensitivity are suggested to receive lower than standard warfarin dosage.
Clopidogrel—CYP2C19 genotype: Clopidogrel is used to prevent blood clots and is often used in combination with aspirin. Clopidogrel is metabolized to its active thiol metabolite, which inhibits platelet activation and aggregation. Deficient CYP2C19 results in enzyme deficiency, leading to decreased concentrations of the active clopidogrel thiol metabolite, which eventually leads to inhibition of platelet activation and aggregation. Individuals inheriting the deficient CYP2C19 variant have an increased risk for adverse cardiovascular events. Pharmacogenomics testing is recommended to assess the patient’s response to the drug. Examples of alternative antiplatelet therapy include Prasugrel and Ticagrelor.
Simvastatin—SLCO1B1 genotype: Statins are used to lower the LDL cholesterol levels by 20%-60% while also reducing inflammation. People who have had a heart attack, stroke, bypass surgery, stents, or diabetes are recommended to take statins. Some patients with a high LDL level without a heart disease are also prescribed statins. Common side effect of statins include myopathy, which limits their use. The SLCO1B1 gene encodes an organic anion polypeptide transporter 1B1 whose function is to transport most of the statins to the liver. The 521T>C (p. Val174Ala) polymorphism leads to myopathy caused by statins. In clinical practice, lower doses of simvastatin or alternatives to statins such as pravastatin or rosuvastatin were used for people with the 521CT or CC genotypes.
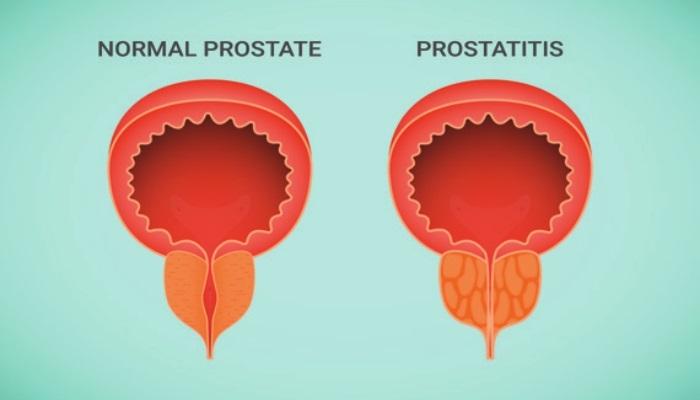
β-blockers—CYP2D6/ADBR1 genotype: Beta-blockers are used to block the effects of adrenaline in response to stressful situations. Beta-blockers are prescribed for the treatment of conditions like angina, heart attacks, congestive heart failure, and abnormal heart rhythms. Beta-blockers are antagonists which compete with catecholamine to bind to β-1-adrenergic receptors (ADBR1). Several genes associated with variation in β-blocker responses include CYP2D6, ADBR1, and ADBR2. CYP2D6 loss-of-function variants have been linked to poor metabolizers of β-blockers such as propranolol, timolol, and metoprolol. About 5–10% of the population carries two or more loss-of-function CYP2D6 alleles. Heart failure patients carrying the mutated CYP2D6 gene may be vulnerable to high drug concentrations and need to be put on alternative medications.
Clopidogrel, warfarin, and simvastatin are examples of how drugs prescribed using pharmacogenomics testing can benefit patients with heart diseases. The desirable aspect of pharmacogenomics testing is the preemptive approach taken by genotyping before the patient receives the drug prescription and dosage, the genetic test results are available in the patient’s records to be utilized by the physicians.
References
- Babayeva, M., Azzi, B., & Loewy, Z. G. (2022). Pharmacogenomics Informs Cardiovascular Pharmacotherapy. Methods in molecular biology (Clifton, N.J.), 2547, 201–240. https://pubmed.ncbi.nlm.nih.gov/36068466/
- Magavern, E. F., Kaski, J. C., Turner, R. M., et al. (2021). The Interface of Therapeutics and Genomics in Cardiovascular Medicine. Cardiovascular drugs and therapy, 35(3), 663–676. https://pubmed.ncbi.nlm.nih.gov/33528719/
- The Big 6 Heart Medications. Cleveland Clinic. https://health.clevelandclinic.org/the-big-six-heart-medications/ Accessed on 21 December 2022.
- Zhou, Z. (2020). Pharmacogenomics in Cardiovascular Precision Medicine. Journal of Laboratory and Precision Medicine, 5, 30-30. https://jlpm.amegroups.com/article/view/5803/html