Pharmacogenomic Evaluation of Chemotherapy Toxicity in Breast Cancer

The outcomes of breast cancer chemotherapeutic management, including response and incidence of adverse events, differ even in patients with similar subtypes, stages, and grades. This variation can be attributed to factors like patient’s age, diet, alcohol use, smoking, menopausal state, other medications, as well as genetic factors. This article discusses the toxicity and adverse events of individual chemotherapeutic agents or combination regimens, investigated through pharmacogenomics studies.
Various classes of cytotoxic agents, such as anthracyclines, taxanes, alkylating agents, antimetabolites, etc. are essential for the treatment of metastatic and some types of early breast cancer. Despite the benefit of chemotherapy in increasing overall survival in breast cancer patients, its side effects affect the treatment outcome.
Anthracycline–induced cardiotoxicity (AIC)
The use of trastuzumab in Her-2 positive cases and left-sided radiation therapy in some cases of left-sided breast cancer are two less-considered cardiotoxicity-disposing factors. Few studies investigating single nucleotide polymorphisms (SNPs) found five SNPs significantly associated with AIC – rs246221 in ABCC1, rs1045642 in ABCB1, rs1056892 in CBR3, rs10838611 in ATG13, and UGT2B7 -161. One study had conflicting results; one variant in CBR3 had no significant association with cardiac failure (Reinbolt et al.). On the other hand, another study showed that this variant significantly increased the risk of reducing the ejection fraction to less than 55% (Hertz et al., 2016). A few other studies found rs28714259 and electron transfer flavoprotein beta (EFTB) gene to be associated with AIC (Schneider et al., 2017 and Ruiz-Pinto et al., 2018)
Taxanes Induced Neuropathy (TIN)
A few studies found that CYP2C8 low function alleles was associated with neurotoxicity following taxane use (Hertz et al., 2013; Abraham et al., 2014; Lam et al., 2016). Two variants of ABCB1, rs1045642 and rs1128503, were found to be associated with an increased risk of neuropathy (Kus et al., 2016; Tanabe et al., 2017), whereas rs3213619 was associated with a decreased risk of sensory neuropathy (Abraham et al., 2014). Low activity alleles in FANCD2 were significantly associated with development of TIN (Sucheston et al., 2011), but this was not replicated in any other cohort. One of the genome-wide association studies suggested a novel biomarker in the congenital peripheral neuropathy gene FGD4 as an effector in the onset of neuropathy, while another indicated that CYP2C8 poor metabolizers are at higher risk of developing grade ≥2 neurotoxicity following paclitaxel treatment (Hertz et al., 2014).

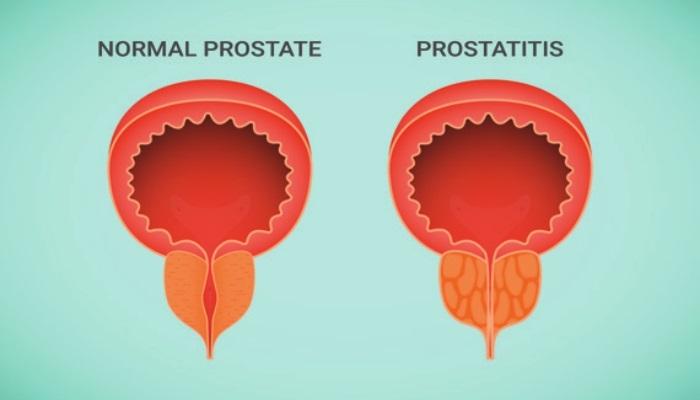
Hematological Toxicity
Hematological toxicity is the most common adverse event that occurs with the use of cytotoxic agents. During chemotherapy, about 50% of breast cancer patients develop neutropenia of any grade, whereas 20% suffer from a more severe form known as febrile neutropenia. A few studies found significant association between ABCB1 variants and hematological toxicity induced by any cytotoxic regimen (Kim et al., 2012; Chaturvedi et al., 2013; Voon et al., 2013; Angelini et al., 2017). The G allele of rs776746 (CYP3A5) showed significant protective effect against neutropenia following any cycle of Adriamycin and cyclophosphamide (Tang et al., 2013). Also, CYP2B6*6 was found to have a protective effect from high grade neutropenia (Tsuji et al., 2016).
Other Systemic Chemotherapy Toxicities
Commonly reported systemic toxicities during breast cancer chemotherapy include nausea, vomiting, diarrhea or constipation, pain, arm swelling, breast skin irritation, and high susceptibility to infections. One study found an SNP, calcium channel voltage-dependent subunit beta 4 (CACNB4), which was associated with docetaxel-induced alopecia. Different pharmacogenomic studies have determined various chemotherapy-associated toxicities in breast cancer patients, but they were not consistent in their selected outcome, their selected genes, and the used chemotherapeutic regimens.
Conclusion
Many breast cancer cases are treated with chemotherapy. Decreasing chemotherapy side effects is essential to improve quality of life of the patients, prevent treatment cessation by practitioners or refusal of treatment by patients. One approach is by pharmacogenomics evaluation of the patient. Recent research has highlighted various genetic variants that are associated with chemotherapeutic toxicity and adverse events.
References:
1. Al-Mahayri ZN, Patrinos GP, Ali BR. Toxicity and Pharmacogenomic Biomarkers in Breast Cancer Chemotherapy. Front Pharmacol. 2020 Apr 15;11:445.
2. Reinbolt R. E., Patel R., Pan X., Timmers C. D., Pilarski R., Shapiro C. L., et al. (2016). Risk factors for anthracycline-associated cardiotoxicity. Support Care Cancer. 24 (5), 2173–2180.
3. Hertz D. L., Caram M. V., Kidwell K. M., Thibert J. N., Gersch C., Seewald N. J., et al. (2016). Evidence for association of SNPs in ABCB1 and CBR3, but not RAC2, NCF4, SLC28A3 or TOP2B, with chronic cardiotoxicity in a cohort of breast cancer patients treated with anthracyclines. Pharmacogenomics 17 (3), 231–240.
4. Schneider B. P., Shen F., Gardner L., Radovich M., Li L., Miller K. D., et al. (2017). Genome-Wide Association Study for Anthracycline-Induced Congestive Heart Failure. Clin. Cancer Res. 23 (1), 43–51.
5. Ruiz-Pinto S., Pita G., Martín M., Alonso-Gordoa T., Barnes D. R., Alonso M. R., et al. (2018). Exome array analysis identifies ETFB as a novel susceptibility gene for anthracycline-induced cardiotoxicity in cancer patients. Breast Cancer Res. Treat 167 (1), 249–256.
6. Hertz D. L., Roy S., Motsinger-Reif A. A., Drobish A., Clark L. S., McLeod H. L., et al. (2013). CYP2C8*3 increases risk of neuropathy in breast cancer patients treated with paclitaxel. Ann. Oncol. 24 (6), 1472–1478.
7. Abraham J. E., Guo Q., Dorling L., Tyrer J., Ingle S., Hardy R., et al. (2014). Replication of genetic polymorphisms reported to be associated with taxane-related sensory neuropathy in patients with early breast cancer treated with Paclitaxel. Clin. Cancer Res. 20 (9), 2466–2475.
8. Eckhoff L., Feddersen S., Knoop A. S., Ewertz M., Bergmann T. K. (2015). Docetaxel-induced neuropathy: a pharmacogenetic case-control study of 150 women with early-stage breast cancer. Acta Oncol. 54 (4), 530–537.
9. Lam S. W., Frederiks C. N., van der Straaten T., Honkoop A. H., Guchelaar H.-J., Boven E. (2016). Genotypes of CYP2C8 and FGD4 and their association with peripheral neuropathy or early dose reduction in paclitaxel-treated breast cancer patients. Br. J. Cancer. 115 (11), 1335–1342.
10. Kus T., Aktas G., Kalender M. E., Demiryurek A. T., Ulasli M., Oztuzcu S., et al. (2016). Polymorphism of CYP3A4 and ABCB1 genes increase the risk of neuropathy in breast cancer patients treated with paclitaxel and docetaxel. Onco Targets Ther. 9, 5073–5080.
11. Tanabe Y., Shimizu C., Hamada A., Hashimoto K., Ikeda K., Nishizawa D., et al. (2017). Paclitaxel-induced sensory peripheral neuropathy is associated with an ABCB1 single nucleotide polymorphism and older age in Japanese. Cancer Chemother. Pharmacol. 79 (6), 1179–1186.
12. Sucheston L. E., Zhao H., Yao S., Zirpoli G., Liu S., Barlow W. E., et al. (2011). Genetic predictors of taxane-induced neurotoxicity in a SWOG phase III intergroup adjuvant breast cancer treatment trial (S0221). Breast Cancer Res. Treat. 130 (3), 993–1002.
13. Hertz D. L., Roy S., Jack J., Motsinger-Reif A. A., Drobish A., Clark L. S., et al. (2014). Genetic heterogeneity beyond CYP2C8*3 does not explain differential sensitivity to paclitaxel-induced neuropathy. Breast Cancer Res. Treat. 145 (1), 245–254.
14. Kim K., Ahn J.-H., Kim S.-B., Jung K. H., Yoon D. H., Lee J. S., et al. (2012). Prospective evaluation of the drug-metabolizing enzyme polymorphisms and toxicity profile of docetaxel in Korean patients with operable lymph node-positive breast cancer receiving adjuvant chemotherapy. Cancer Chemother. Pharmacol. 69 (5), 1221–1227.
15. Chaturvedi P., Tulsyan S., Agarwal G., Lal P., Agarwal S., Mittal R. D., et al. (2013). Influence of ABCB1 genetic variants in breast cancer treatment outcomes. Cancer Epidemiol. 37 (5), 754–761.
16. Voon P. J., Yap H. L., Ma C-Y-T, Lu F., Wong A. L. A., Sapari N. S., et al. (2013). Correlation of aldo-ketoreductase (AKR) 1C3 genetic variant with doxorubicin pharmacodynamics in Asian breast cancer patients. Br. J. Clin. Pharmacol. 75 (6), 1497–1505.
17. Angelini S., Botticelli A., Onesti C. E., Giusti R., Sini V., Durante V., et al. (2017). Pharmacogenetic Approach to Toxicity in Breast Cancer Patients Treated with Taxanes. Anticancer Res. 37 (5), 2633–2639.
18. Tang N. L. S., Liao C. D., Wang X., Mo F. K. F., Chan V. T. C., Ng R., et al. (2013). Role of pharmacogenetics on adjuvant chemotherapy-induced neutropenia in Chinese breast cancer patients. J. Cancer Res. Clin. Oncol. 139 (3), 419–427.
19. Tsuji D., Chaturvedi P., Agarwal G., Lal P., Agrawal S., Mittal R. D., et al. (2013). Pharmacogenetic influence of GST polymorphisms on anthracycline-based chemotherapy responses and toxicity in breast cancer patients: a multi-analytical approach. Mol. Diagn. Ther. 17, 371–379.