Treatments Focus
Is Lung Cancer Genetic? What Experts Know So Far
Cancer of late, has emerged as a vast disease affecting millions of people worldwide. It is
characterised by uncontrolled growth of abnormal cells, forming tumours or invading other
tissues.There are various types of cancer, each with its own set of risk factors, symptoms
and treatment options.
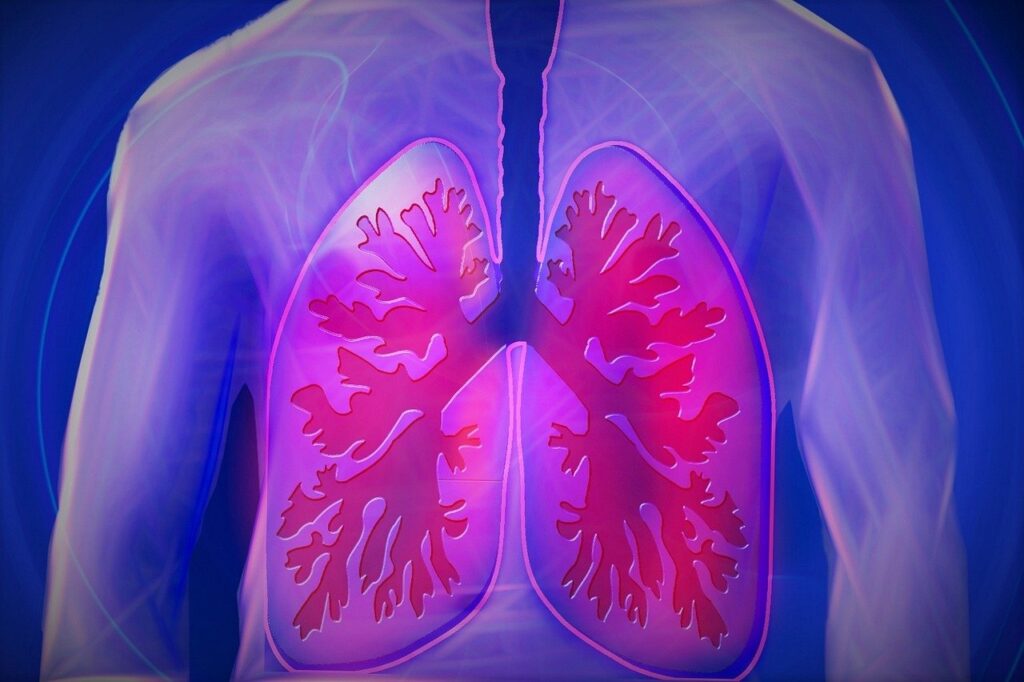
One particular type of cancer that poses a significant health challenge is lung cancer. It is
the leading cause of cancer related deaths worldwide. It affects the cell linings in the air
passage of lungs. Though lung cancer is often primarily associated with smoking, the
majority of smokers do not develop lung cancer and many patients with lung cancer have
never smoked. Does it mean that there is a relationship between lung cancer and genetics?
Well, a family history of lung cancer increases the risk of the disease for both smokers and
non-smokers.
Case Study on Inherited lung cancer
A Japanese descent was reported with inherited lung cancer. At the time of analysis, the 53
year old female was diagnosed with multiple lung adenocarcinomas in the bilateral lungs.
She was a light smoker with a 1.2-pack-year history of smoking. Her mother, who was a
never smoker, also suffered from multiple lung adenocarcinomas. On performing exome
sequencing using tumour and blood samples of affected and non-family members, novel
germline mutations were detected in the females of the family. The tests revealed the
possibility that germline mutations target female never smokers. This case study led to a
conclusion that oncogenes may cause genetic lung cancer.
Hence, genetic history, radiation exposure and environmental pollution are the main factors
involved in the development of lung cancer.
Genetic factors of Lung Cancer
Genetic factors significantly contribute to the development of sporadic lung cancer. There is an interplay between the inherited traits and acquired mutations which contributes to the
initiation and progression of lung cancer. Having certain genetic mutations directly associated with the development of lung cancer, a major chunk of them are linked to Non-small cell lung cancer(NSCLC), especially lung adenocarcinoma, as opposed to Small cell lung cancers(SCLC). Malignant tumours develop due to the mutations in a particular gene, which grows uncontrollably and may invade other tissues.
EGFR gene.
Analysing specific genes like EGFR(Epidermal Growth Factor Receptor) and their mutations
confirms their significant role fueling the growth of lung tumours. They can be identified both in primary tumours and in metastases(secondary tumours that have spread to distant sites).These mutations tend to mutate rapidly and often react resistant to the drugs used to treat them.
KRAS gene.
KRAS encodes a G-protein that controls signalling pathways regulating cell proliferation,
differentiation and survival. Activating mutations in the KRAS oncogene are most commononcogene alterations in lung-adenocarcinoma, occurring in 25-40% of cases. Interestingly, KRAS mutations are more frequently observed in Western populations than in Asian populations, and in male smokers than in female smokers.
TP53 gene.
Lung Cancer: Genetic disease or Environmental disaster?
The impact of lifestyle choices on lung cancer risk in genetically predisposed individuals can
be fatal. Environmental factors responsible for lung cancer include air pollution, exposure to
carcinogenic chemicals and alcohol consumption. Other than that, exposure to radon, heavy metals used in smelting and asbestos increase the risk of developing cancer.
Smoking as a causing factor.
Smoking is perceived as a major cause of cancer; however, only a fraction of long term
smokers develop lung cancer. The development of cancer depends on how long an
individual has smoked in addition to other causes of cancer. Tobacco smoke comprises
polycyclic aromatic hydrocarbons (PAH) which are common DNA-damaging carcinogens.
These PAHs interact with DNA and form mutagenic DNA abducts, which triggers the onset
of lung cancer.
Air pollution.
The emissions from the vehicles, factories, industrial plants and agriculture contribute to the
risk of respiratory and cardiovascular diseases. Furthermore, incomplete combustion of
wood or fuel from industrial or vehicles leads to rise in carcinogens like PAH. Long term
exposure of PAH leads to an increase in the incidents of lung cancer.
Also, long term exposure to gases like nitrogen oxide, nitrogen dioxide and sulphur dioxide
increases the lung cancer associated mortality rate.
Genetic testing for Lung Cancer.
A family history of lung cancer increases the risk of the disease for both smokers and non-
smokers. Genetic test for lung cancer involves Next generation sequencing(NGS), which
makes it possible to perform comprehensive analysis of the genome at high speed. This
helps to identify the causative genes, which further results in elucidating carcinogenesis of
lung cancer as well as in developing new therapeutic strategies of lung cancer.
Genetic Lung Cancer Survival Rates.
When detected at an early age, it can be treated surgically, with a good survival rate;
however most cases are identified at a late stage when surgery is no longer an option due to distant metastases. Germline EGFR mutations cause rare and characteristic inherited lung cancer syndromes,
which target non-smokers, especially the females. Although the cases of genetic lung
cancers are rare, it is necessary for the unaffected family members to go for the tests as
they have an increased risk to develop lung cancer. The molecular characteristics may
contribute to understanding the pathogenesis of lung cancer, and thus they may also shed
light on elucidation of sporadic lung cancer.
Conclusion.
In conclusion, while lifestyle choices and environmental factors contribute primarily to lung
cancer, the assumption that lung cancer is genetically linked can’t be ignored.
Understanding the interplay between the genetic predisposition and environmental factors,
We the best genetic testing company in India is “GenePowerX” develop targeted prevention
strategies and personalised treatments for individuals at risk of or diagnosed with lung
cancer. Advancement in genetic testing continues to offer promising avenues for early
detection and tailored therapies, ultimately improving outcomes for those affected by the
disease.
Sources By
Related Articles
Book an Appointment to understand how GenepoweRx can help you in treating
Is Lung Cancer Genetic? What Experts Know So Far
Meet The Doctors
Dr Kalyan Uppaluri
Dr Hima Challa
Your genetics … Your Test ... Your Health Success
It’s always the word of mouth that’s the best advice. Here are some of our…
Our Partners





Professional Partnerships
Government Association